When it comes to treating illness, one-size-fits-all doesn’t work. Men and women don’t just differ in biology-they respond differently to medications, recover at different rates, and even show symptoms in unique ways. Yet for decades, medical research treated male bodies as the default. That’s changing. Today, gender-specific treatment approaches are proving to save lives, reduce side effects, and improve outcomes across conditions from heart disease to depression.
Why Gender Matters in Treatment
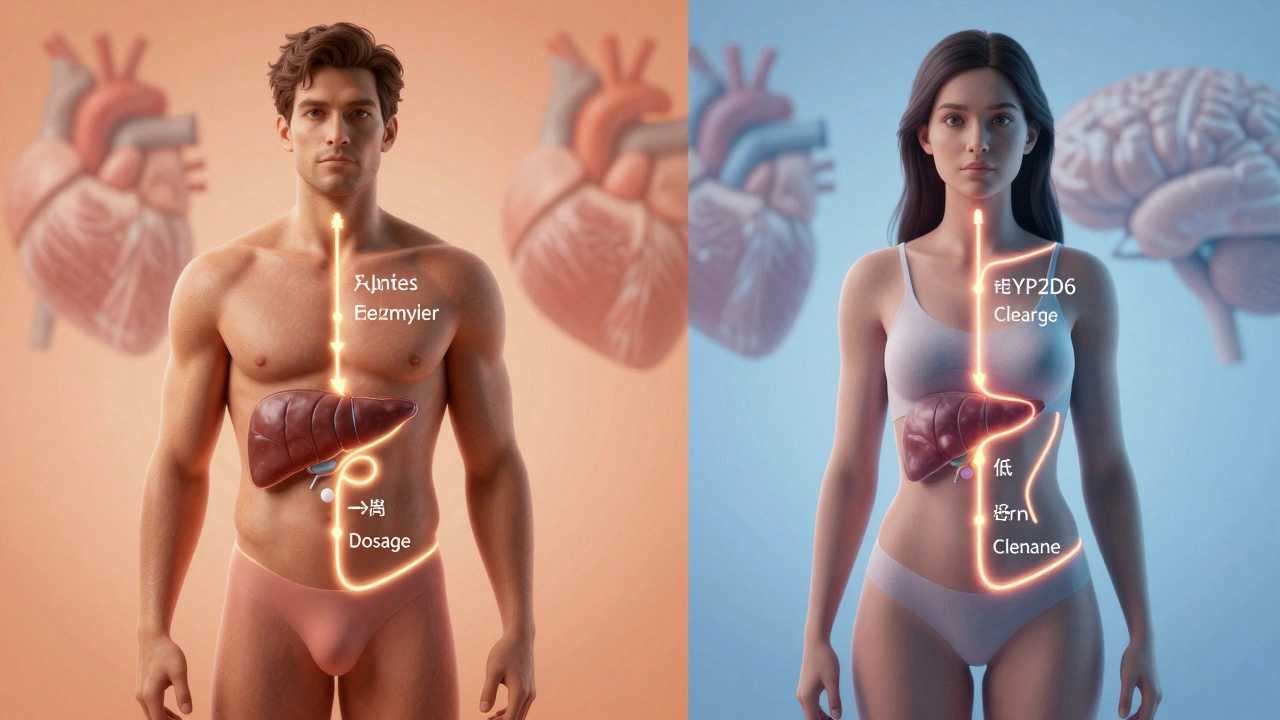
Biological differences between males and females go far beyond hormones. Men and women have different body compositions, liver enzyme activity, fat distribution, and even brain chemistry. These aren’t minor details-they directly affect how drugs are absorbed, metabolized, and eliminated.
Take antidepressants. A 2023 study from the Mayo Clinic found that women respond better to SSRIs like sertraline, while men show stronger improvement with SNRIs like venlafaxine. Why? Women have higher levels of the enzyme CYP2D6, which breaks down certain drugs faster. That means a standard dose for men might be too weak for a woman, and vice versa.
Heart attacks tell another story. Men often have classic chest pain. Women? They’re more likely to report fatigue, nausea, jaw pain, or back discomfort. Because emergency rooms historically trained staff to look for the male symptom profile, women were misdiagnosed up to 50% more often in the 1990s. Even today, some providers still overlook these signs.
Cardiovascular Disease: Different Risks, Different Treatments
Heart disease is the leading killer of both men and women. But it doesn’t strike them the same way. Men typically develop plaque buildup in larger arteries. Women often have microvascular disease-tiny vessel damage that doesn’t show up on standard angiograms.
That’s why women with chest pain but normal heart scans are frequently told it’s stress or anxiety. But studies now confirm: their symptoms are real. Treatment for women often includes anti-inflammatory drugs, blood pressure control, and lifestyle changes focused on metabolic health, not just cholesterol-lowering statins.
Aspirin use also differs. For men, daily low-dose aspirin reduces heart attack risk by 32%. For women? It cuts stroke risk by 17% but doesn’t significantly lower heart attack rates. Guidelines now recommend aspirin for men over 50 with risk factors, but only for women with a clear history of cardiovascular events.
Mental Health: Hormones, Trauma, and Therapy
Depression affects twice as many women as men. But that doesn’t mean men are less affected-they just express it differently. Men are more likely to turn to alcohol, work obsessively, or become irritable. They’re also far more likely to die by suicide, even though women attempt it more often.
Therapy approaches reflect this. Women often benefit from talk therapies that explore emotional patterns, relationships, and self-worth. Cognitive Behavioral Therapy (CBT) works well here. Men respond better to action-based strategies: problem-solving, physical activity, and skill-building. Group therapy for men often focuses on rebuilding confidence through competence, not just talking about feelings.
Hormonal shifts also play a role. Postpartum depression isn’t just about baby blues. Fluctuations in estrogen and progesterone after childbirth can trigger chemical imbalances that last months. Treatment often combines therapy with hormone monitoring, not just antidepressants.
Chronic Pain: The Gender Gap in Diagnosis
Women are 30% more likely to suffer from chronic pain conditions like fibromyalgia, migraines, and arthritis. But they’re also 40% less likely to get adequate pain relief. Why? Studies show doctors tend to underestimate women’s pain reports, assuming emotional factors are to blame.
Men, on the other hand, are more likely to be prescribed opioids for back pain-even when physical therapy would be safer. Women are more often pushed toward antidepressants or anti-seizure meds like gabapentin, which work better for nerve-related pain.
Research from the National Institutes of Health in 2025 found that women process pain signals differently in the brain. Their nervous systems are more sensitive to inflammation. That’s why treatments targeting inflammation-like omega-3 supplements, low-dose naltrexone, and yoga-are showing better results for women than traditional painkillers.
Medication Dosing: The Missing Variable
Most drug dosages are still based on trials done mostly on men. That’s changing, but slowly. In 2024, the FDA updated guidelines requiring sex-specific data in Phase 3 trials for new drugs. Still, thousands of older medications remain unadjusted.
For example, the sleep drug zolpidem (Ambien). Women clear it from their bloodstream slower than men. The FDA now recommends half the dose for women. Many doctors still don’t know this. The same goes for statins, anticoagulants, and even insulin.
Doctors who use gender-specific dosing see fewer side effects. Women on lower doses report less dizziness, fatigue, and liver stress. Men on higher doses (when appropriate) get better control of their condition without increased risk.

Prevention and Screening: Tailored Strategies
Screening protocols are starting to catch up. Men over 50 get prostate cancer screenings. Women get mammograms and Pap smears. But what about other conditions?
Men are more likely to die from liver disease, often because they delay care. Screening for fatty liver disease with ultrasound and blood tests is now recommended for men over 40 with obesity or alcohol use. Women are more likely to develop autoimmune disorders-lupus, rheumatoid arthritis, Hashimoto’s. Regular thyroid and ANA testing after age 35 can catch these early.
Prevention isn’t just about tests. Men benefit more from strength training to reduce heart risk. Women benefit more from weight-bearing exercise and vitamin D to protect bone density. Diet matters too: women need more iron and folate; men need more magnesium and zinc.
What’s Next? The Future of Gender-Specific Care
Gender-specific treatment isn’t about dividing care into male and female boxes. It’s about recognizing that biology, environment, and behavior shape health differently. The goal isn’t to treat men and women as opposites-but as distinct subgroups with unique needs.
AI is helping. New algorithms analyze patient data by sex, age, and hormone levels to predict drug reactions. Clinics in Minnesota and California now use these tools to personalize prescriptions in real time. Early results show 30% fewer adverse events and 20% faster recovery.
Patients should ask: "Does this treatment consider my sex?" If the answer is no, push for more information. You’re not being difficult-you’re being smart.
Key Takeaways
- Men and women metabolize drugs differently-dosing should reflect that.
- Symptoms of heart disease, depression, and chronic pain vary by gender.
- Screening and prevention strategies need to be sex-specific, not one-size-fits-all.
- Therapy approaches work better when matched to how each gender expresses distress.
- Always ask if your treatment plan considers your biological sex-not just your diagnosis.
Are gender-specific treatments only for physical health?
No. Gender-specific approaches apply to mental health, chronic pain, medication dosing, and even preventive care. Women respond differently to therapy for depression, while men often need different strategies to manage anxiety or anger. Treatment isn’t just about pills-it’s about how your body, mind, and life experiences interact.
Is gender-specific treatment the same as sex-based treatment?
Not exactly. "Sex" refers to biological traits like chromosomes, hormones, and anatomy. "Gender" includes social, cultural, and psychological factors. In medicine, most guidelines focus on biological sex because those differences are measurable and directly impact physiology. But gender identity can influence care access, communication with providers, and willingness to seek help. The best care considers both.
Why aren’t all doctors using gender-specific treatments yet?
Many doctors were trained before this research became mainstream. Medical textbooks still often use male-only data. Plus, time and resources are limited in clinics. But awareness is growing. The FDA, CDC, and major medical associations now require sex-disaggregated data in research. As newer doctors enter practice and AI tools become common, this will become standard.
Can gender-specific treatment help non-binary or transgender patients?
Yes, but differently. For transgender patients, hormone therapy changes how drugs are processed. A transgender woman on estrogen may metabolize medications like a cisgender woman. A transgender man on testosterone may respond more like a cisgender man. The key is knowing their current hormone levels and medical history-not their assigned sex at birth. Providers who use individualized, hormone-informed care see better outcomes for all patients.
What should I ask my doctor about gender-specific treatment?
Ask: "Is this treatment based on data from people like me?" If you’re a woman, ask if the dosage was tested on women. If you’re a man, ask if the symptoms you’re experiencing are typical. Request to see the research behind the recommendation. You have a right to know whether your care is tailored to your biology-not just your diagnosis.